Question 1
A patient has gained 8 kg in the past week. Serum sodium is 115 mEq/L, CVP is 20 mm Hg, and serum
osmolality is decreased. The patient has just experienced a generalized tonic-clonic seizure. In this
situation, which of the following IV solutions should a nurse be prepared to administer?
- A. 3% sodium chloride
- B. 0.45% sodium chloride
- C. 0.9% sodium chloride
- D. 5% dextrose with 0.25% sodium chloride
Answer:
A
Explanation:
The patient has signs of severe hyponatremia, which is a low level of sodium in the blood.
Hyponatremia can cause cerebral edema, which can lead to seizures, confusion, coma, and death.
The patient needs a hypertonic solution, which is a fluid that has a higher concentration of solutes
than the blood, to draw water out of the brain cells and restore the normal sodium level. 3% sodium
chloride is a hypertonic solution that can be used to treat severe hyponatremia. 0.45% sodium
chloride, 0.9% sodium chloride, and 5% dextrose with 0.25% sodium chloride are all hypotonic
solutions, which are fluids that have a lower concentration of solutes than the blood, and would
worsen the patient’s condition by adding more water to the blood and the brain.
Reference:
AACN. (2023). CCRN (Adult) Exam Handbook. Retrieved from [CCRN Exam Handbook], p. 18.
AACN. (2023). CCRN (Adult) Exam Blueprint. Retrieved from [CCRN Exam Blueprint], p. 2.
AACN. (2020). Practice Alert: Hyponatremia. Retrieved from [Practice Alert], p. 1-2.
Lewis, S. L., Bucher, L., Heitkemper, M. M., Harding, M. M., Kwong, J., & Roberts, D. (2017). Medical-
surgical nursing: Assessment and management of clinical problems (11th ed.). St. Louis, MO: Elsevier.
Retrieved from [Textbook], p. 303-304.
Comments
Question 2
A patient who experienced a blunt chest trauma in an automobile crash is admitted with multiple rib
fractures. The patient is dyspneic and hypotensive and is reporting left shoulder pain. On
auscultation, a nurse notes that bowel sounds can be heard over the lower left thorax. These findings
are consistent with
- A. ruptured abdominal viscus.
- B. ruptured diaphragm.
- C. flail chest.
- D. mediastinal shift.
Answer:
B
Explanation:
The patient’s findings are consistent with a ruptured diaphragm, which is a tear in the muscle that
separates the chest and abdominal cavities. A blunt chest trauma can cause a sudden increase in
intra-abdominal pressure, which can rupture the diaphragm and allow abdominal organs to herniate
into the thorax. This can cause dyspnea, hypotension, shoulder pain, and bowel sounds over the
lower thorax. A ruptured abdominal viscus would cause peritonitis, which would present with
abdominal pain, distension, fever, and signs of sepsis. A flail chest would cause paradoxical chest
movement, respiratory distress, and cyanosis. A mediastinal shift would cause tracheal deviation,
decreased breath sounds, and jugular venous distension.
Reference:
AACN. (2023). CCRN (Adult) Exam Handbook. Retrieved from [CCRN Exam Handbook], p. 18.
AACN. (2023). CCRN (Adult) Exam Blueprint. Retrieved from [CCRN Exam Blueprint], p. 2.
BCEN. (2020). Trauma Certified Registered Nurse (TCRN) Examination Content Outline. Retrieved
from [TCRN Exam Content Outline], p. 8.
Lewis, S. L., Bucher, L., Heitkemper, M. M., Harding, M. M., Kwong, J., & Roberts, D. (2017). Medical-
surgical nursing: Assessment and management of clinical problems (11th ed.). St. Louis, MO: Elsevier.
Retrieved from [Textbook], p. 1789-1790.
Comments
Question 3
The goal of PEEP therapy in acute lung injury (ALI) is to
- A. decrease PAP.
- B. decrease airway resistance.
- C. increase cardiac output.
- D. reduce physiologic shunting.
Answer:
D
Explanation:
The goal of PEEP therapy in acute lung injury (ALI) is to reduce physiologic shunting, which is the
perfusion of blood through unventilated or collapsed alveoli. This results in hypoxemia and impaired
gas exchange. PEEP therapy increases the end-expiratory pressure and prevents alveolar collapse,
thus improving ventilation and oxygenation. PEEP therapy does not necessarily decrease PAP
(pulmonary artery pressure), decrease airway resistance, or increase cardiac output. In fact, PEEP
therapy may have adverse effects on these parameters, such as increasing intrathoracic pressure,
reducing venous return, and decreasing cardiac output.
Reference:
AACN. (2023). CCRN (Adult) Exam Handbook. Retrieved from [CCRN Exam Handbook], p. 18.
AACN. (2023). CCRN (Adult) Exam Blueprint. Retrieved from [CCRN Exam Blueprint], p. 2.
AACN. (2020). Practice Alert: Acute Lung Injury/Acute Respiratory Distress Syndrome. Retrieved from
[Practice Alert], p. 1-2.
Lewis, S. L., Bucher, L., Heitkemper, M. M., Harding, M. M., Kwong, J., & Roberts, D. (2017). Medical-
surgical nursing: Assessment and management of clinical problems (11th ed.). St. Louis, MO: Elsevier.
Retrieved from [Textbook], p. 1908-1910.
Comments
Question 4
A patient's blood culture report notes the presence of vancomycin resistant enterococcus. The nurse
should place the patient in which type of isolation?
- A. droplet
- B. airborne
- C. contact
- D. protective
Answer:
C
Explanation:
The nurse should place the patient in contact isolation, which is a type of precaution used to prevent
the transmission of microorganisms that are spread by direct or indirect contact with the patient or
the patient’s environment. Contact isolation requires the use of gloves and gowns when entering the
patient’s room, as well as dedicated patient-care equipment and proper hand hygiene. Vancomycin
resistant enterococcus (VRE) is a type of bacteria that is resistant to the antibiotic vancomycin and
can cause infections in various sites, such as the urinary tract, bloodstream, or wounds. VRE can be
spread by contact with contaminated surfaces, equipment, or hands.
Reference:
AACN. (2023). CCRN (Adult) Exam Handbook. Retrieved from [CCRN Exam Handbook], p. 18.
AACN. (2023). CCRN (Adult) Exam Blueprint. Retrieved from [CCRN Exam Blueprint], p. 2.
CDC. (2019). Guidelines for Isolation Precautions: Preventing Transmission of Infectious Agents in
Healthcare Settings. Retrieved from [CDC Guidelines], p. 69-70.
CDC. (2019). Vancomycin-resistant Enterococci (VRE) and the Clinical Laboratory. Retrieved from
[CDC Fact Sheet], p. 1-2.
Comments
Question 5
A nurse has responded to a rapid response call on a medical-surgical floor in the hospital. The nurse
finds the patient with the following data:
BP
72/30
HR
132
RR
T
102.3° F (39.0° C)
SpO2 95%
Ph
7.13
PaCO2 34 mm Hg
PaO2 88 mm Hg
HCO3 14 mEq/L
Na+ 142 mEq/L
The nurse should anticipate an order to administer which of the following?
- A. 8.4% sodium bicarbonate
- B. phenylephrine (Neo-Synephrine)
- C. 0.9% sodium chloride
- D. amiodarone (Cordarone)
Answer:
B
Explanation:
The patient’s data indicate that the patient is in shock, which is a life-threatening condition
characterized by inadequate tissue perfusion and organ dysfunction. The patient has a low blood
pressure, a high heart rate, a fever, and a metabolic acidosis, which suggest that the patient may
have septic shock, which is caused by a severe infection that triggers a systemic inflammatory
response. The nurse should anticipate an order to administer phenylephrine (Neo-Synephrine),
which is a vasopressor agent that constricts the blood vessels and increases the blood pressure and
tissue perfusion.
Phenylephrine is recommended as a first-line agent for septic shock by the
Surviving Sepsis Campaign guidelines1
.
8.4% sodium bicarbonate is not indicated for the treatment
of septic shock, as it may worsen the acid-base balance and increase the risk of complications2
.
0.9%
sodium chloride is a normal saline solution that may be used for fluid resuscitation, but it may not be
sufficient to restore the blood pressure and may cause fluid overload, hyperchloremia, and kidney
injury3
.
Amiodarone (Cordarone) is an antiarrhythmic drug that is used to treat ventricular
tachycardia or fibrillation, but it is not effective for septic shock and may cause hypotension,
bradycardia, and other adverse effects4
.
Reference:
Surviving Sepsis Campaign. (2020). Surviving Sepsis Campaign: Guidelines on the Management of
Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Retrieved from
, p. 16.
Marik, P. E., & Bellomo, R. (2013). A rational approach to fluid therapy in sepsis. British Journal of
Anaesthesia, 110(3), 323-329. Retrieved from
, p. 327.
Semler, M. W., & Rice, T. W. (2019). Saline versus balanced crystalloids for intravenous fluid therapy
in the emergency department: study protocol for a cluster-randomized, multiple-crossover trial.
Trials, 20(1), 1-10. Retrieved from
, p. 2-3.
Lexicomp Online. (2021). Amiodarone. Retrieved from
, p. 1-2.
Comments
Question 6
Which of the following is most indicative of successful treatment for salicylate poisoning?
- A. osmotic diuresis
- B. decrease in gastric pH
- C. decrease in CPK
- D. alkalinization of urine
Answer:
D
Explanation: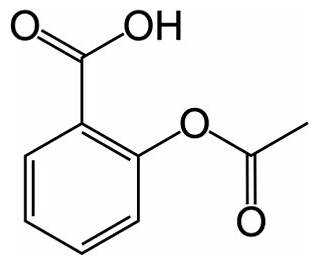
Alkalinization of urine is one of the main goals of treatment for salicylate poisoning, as it enhances
the renal excretion of salicylate and reduces its reabsorption. Alkalinization of urine can be achieved
by administering intravenous sodium bicarbonate and maintaining adequate hydration and urine
output. Alkalinization of urine can be monitored by measuring the urine pH, which should be above
7.5. Osmotic diuresis, decrease in gastric pH, and decrease in CPK are not indicative of successful
treatment for salicylate poisoning. Osmotic diuresis may occur as a result of salicylate toxicity, but it
does not improve the elimination of salicylate. Decrease in gastric pH may impair the absorption of
salicylate, but it does not affect the elimination of salicylate. Decrease in CPK may reflect the
resolution of rhabdomyolysis, which is a possible complication of salicylate poisoning, but it does not
reflect the clearance of salicylate.
Reference:
Salicylate (aspirin) poisoning: Management - UpToDate1
, p. 1-2.
Salicylate poisoning - Symptoms, diagnosis and treatment | BMJ Best Practice US2
, p. 4-5.
Comments
Question 7
A patient is admitted for sepsis secondary to pneumoni
a. The patient has received 2000 mL of plasmalyte and their BP remains 80/50. What should the
nurse anticipate next for the patient?
- A. dopamine
- B. norepinephrine
- C. 1L of plasmalyte
- D. vasopressin
Answer:
B
Comments
Question 8
A patient with a sodium level of 114 mEq/L is most likely to develop
- A. tetany.
- B. flaccid paralysis.
- C. seizures.
- D. cardiac arrhythmias.
Answer:
C
Explanation:
A patient with a sodium level of 114 mEq/L is most likely to develop seizures, which are a
manifestation of severe hyponatremia and cerebral edema. Hyponatremia is a low level of sodium in
the blood, which can cause water to move into the brain cells and cause them to swell. This can lead
to increased intracranial pressure, neurological dysfunction, and seizures. Seizures are a medical
emergency and require prompt treatment to prevent brain damage or death. Tetany, flaccid
paralysis, and cardiac arrhythmias are not typical signs of hyponatremia, but may occur in other
electrolyte disorders, such as hypocalcemia, hyperkalemia, or hypokalemia.
Reference:
Overview of the treatment of hyponatremia in adults - UpToDate1
, p. 1-2.
Manifestations of hyponatremia and hypernatremia in adults - UpToDate2
, p. 1-2.
Comments
Question 9
A patient with a history of six cardiac catheterizations relates that he has received differing
instructions about the duration of required bedrest after the procedure. To further investigate this
issue, which of the following is a nurse's most appropriate action?
- A. Ask about obtaining an independent evaluation of unit outcomes.
- B. Conduct an informal chart review and outcome evaluation of patients treated with different bedrest protocols.
- C. Review recent published research about bedrest protocols.
- D. Ask the nursing supervisor to request standardized physician orders for patients who have undergone catheterization.
Answer:
C
Explanation:
The nurse’s most appropriate action is to review recent published research about bedrest protocols,
as this would provide the nurse with the most current and reliable evidence to guide clinical practice
and improve patient outcomes. Bedrest protocols after cardiac catheterization may vary depending
on the type of access site, the use of closure devices, the patient’s risk factors, and the clinician’s
preference.
However, there is a growing body of research that supports early ambulation and shorter
bedrest duration to reduce the risk of complications, such as bleeding, hematoma, back pain, and
venous thromboembolism, and to enhance patient comfort and satisfaction123
. Asking about
obtaining an independent evaluation of unit outcomes, conducting an informal chart review and
outcome evaluation of patients treated with different bedrest protocols, or asking the nursing
supervisor to request standardized physician orders for patients who have undergone catheterization
are not the most appropriate actions, as they may not reflect the best available evidence, may be
biased or incomplete, or may not address the patient’s concern.
Reference:
1: Bedrest After Cardiac Catheterization: A Systematic Review and Meta-analysis4
, p. 1-2.
: Early Ambulation After Cardiac Catheterization: A Literature Review, p. 1-2.
: Bed Rest After Cardiac Catheterization: A Review of the Evidence, p. 1-2.
Comments
Question 10
A patient is 2 days post MI. The patient was stable until this morning, when severe chest discomfort
developed. Assessment reveals:
BP
70/palpable
HR
122
RR
PAOP 28 mm Hg, with large V waves
CI
1.6 L/min/m2
Cool, clammy skin
Inspiratory crackles throughout the lung field
Loud blowing holosystolic murmur at the apex
The patient's present clinical status is most likely a result of
- A. papillary muscle rupture.
- B. cardiac tamponade.
- C. acute aortic insufficiency.
- D. ventricular septal defect.
Answer:
D
Explanation:
The patient’s present clinical status is most likely a result of a ventricular septal defect (VSD), which is
a hole in the wall between the left and right ventricles. A VSD can occur as a mechanical
complication of MI, usually within the first week, due to necrosis and rupture of the ventricular
septum. A VSD causes a left-to-right shunt of blood, which leads to increased pulmonary pressure,
pulmonary edema, and reduced cardiac output. The patient’s symptoms and signs are consistent
with a VSD, such as severe chest pain, hypotension, tachycardia, respiratory distress, high PAOP with
large V waves, low CI, cool and clammy skin, inspiratory crackles, and a loud blowing holosystolic
murmur at the apex. A papillary muscle rupture, a cardiac tamponade, and an acute aortic
insufficiency are other possible mechanical complications of MI, but they have different clinical
manifestations.
A papillary muscle rupture causes acute mitral regurgitation, which presents with a
soft systolic murmur at the apex and pulmonary congestion1
.
A cardiac tamponade causes
compression of the heart by pericardial fluid, which presents with hypotension, muffled heart
sounds, and jugular venous distension2
.
An acute aortic insufficiency causes backflow of blood from
the aorta to the left ventricle, which presents with a diastolic decrescendo murmur at the left sternal
border and a wide pulse pressure3
.
Reference:
1: Mechanical complications of acute myocardial infarction - UpToDate4
, p. 2-3.
: Cardiac tamponade - Symptoms, diagnosis and treatment | BMJ Best Practice US, p. 1-2.
: Acute aortic regurgitation - Symptoms, diagnosis and treatment | BMJ Best Practice US, p. 1-2.
Comments
Page 1 out of 14
Viewing questions 1-10 out of 150
page 2